Unless you work for an insurance company, you probably do not spend a lot of your time studying all the terminology that dental insurance companies use to describe the treatments and services they cover. If it seems pretty confusing, here are some of the most commonly used dental insurance terms and what they mean.
A Basic Glossary
Annual Maximum–The maximum amount your policy will pay per year for care at North Pole Dental Workshop. It is often divided into costs per individual, and (if you are on a family plan) per family
Co-payment– An amount the patient pays at the time of service before receiving care, and before the insurance pays for any portion of the care
Covered Services– A list of all the treatments, services, and procedures the insurance policy will cover under your contract
Deductible– A dollar amount that you must pay out of pocket each year before the insurance company will pay for any treatments or procedures
Diagnostic/Preventive Services– A category of treatments or procedures that most insurance will cover before the deductible which may include services like preventive appointments with Dr. Bauer, X-rays, and evaluations
In-Network and Out-of-Network– A list of providers that are part of an insurance company’s “network”
- If you visit in-network providers, the insurance company will typically cover a larger portion of the cost of the care you receive. If you visit someone who is not part of the network, known as an out-of-network provider, the insurance company may pay for a portion of the care, but you will pay a significantly larger share from your own pocket.
Lifetime Maximum– The maximum amount that an insurance plan will pay toward care for an individual or family (if you have an applicable family plan)
- This is not a per-year maximum, but rather a maximum that can be paid over the entire life of the patient.
Limitations/Exclusions– A list of all the procedures an insurance policy does not cover
- Coverage may limit the timing or frequency of a specific treatment or procedure (only covering a certain number within a calendar year), or may exclude some treatments entirely. Knowing the limitations and exclusions of a policy is very important.
Member/Insured/Covered Person/Beneficiary/Enrollee– Someone who is eligible to receive benefits under an insurance plan
Provider– Dr. Bauer or other oral health specialist who provides treatment
Waiting Period– A specified amount of time that the patient must be enrolled with an insurance plan before it will pay for certain treatments; waiting periods may be waived if you were previously enrolled in another dental insurance plan with a different carrier
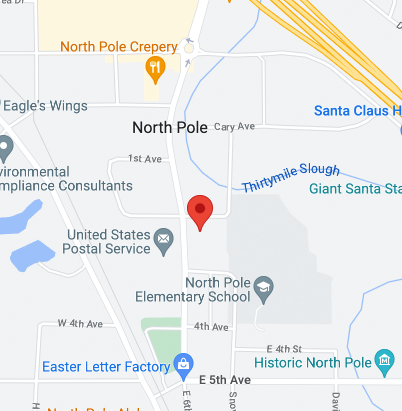
There are many different insurance options available, so you need to find out exactly what your insurance covers. It’s important to review your plan with a qualified insurance specialist. Don’t be afraid to ask questions about the policy so you can understand it fully and be confident that you know everything your policy covers the next time you come in for treatment at our North Pole office.